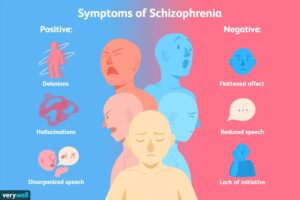
BY HUMAIRA HASAN, PALAK, AND UPASANA KOUL INTRODUCTION WHAT IS SCHIZOPHRENIA? Schizophrenia is a serious brain disorder affecting around 1% of the global population and is one of the top 10 causes of disability worldwide (Marder & Cannon, 2019). This condition is characterized by symptoms such as hallucinations (e.g., seeing or hearing things that aren’t there), delusions (false beliefs), disorganized speech, and abnormal behavior. Additionally, individuals with schizophrenia often experience a lack of motivation, reduced emotional expression, and cognitive difficulties, including problems with thinking, memory, and decision-making (Jauhar, Johnstone, & McKenna, 2022). The impact on daily life can be significant, leading to severe disability and incomplete recovery. Even individuals who show improvement may still struggle with social isolation, stigma, and limited opportunities for building close relationships. Unemployment rates are high among those with schizophrenia, and lifestyle factors such as poor diet, weight gain, smoking, and substance use contribute to a reduced life expectancy of 13 to 15 years (Hjorthøj, Stürup, McGrath, & Nordentoft, 2017; Kahn, 2020). The lifetime risk of death by suicide for individuals with schizophrenia ranges from 5% to 10% (McCutcheon, Reis Marques, & Howes, 2020). Current diagnosis and treatment primarily target psychotic symptoms, but negative and cognitive symptoms are equally important due to their significant impact on social and professional functioning. These symptoms often do not respond well to conventional antipsychotic medications (Kahn, 2020; Jauhar, Johnstone, & McKenna, 2022). Historically, schizophrenia was conceptualized by Emil Kraepelin as “dementia praecox,” a term later renamed “schizophrenia” by Eugen Bleuler. Notably, both Kraepelin and Bleuler did not consider positive symptoms like delusions and hallucinations as the primary characteristics of the disorder. This historical perspective supports the view that a more comprehensive approach is needed for understanding and treating schizophrenia (Kahn, 2020). PREVALENCE AND ONSET Schizophrenia is a genetic neurocognitive disorder that affects approximately 1% of the population, typically appearing between the ages of 21 and 25 in males and 25 and 30 in females. (Zhan et al., 2023) Extensive research suggests that from 1990 to 2019, global schizophrenia cases rose by over 65%, new diagnoses by 37%, and health impacts (DALYs) by 65%, while age-adjusted rates stayed stable. (Solmi et al., 2023) TREATMENT Schizophrenia treatment is lifelong and combines medications with psychosocial support, guided by a psychiatrist and a care team. Antipsychotic medications, including both first- and second-generation options, are the primary treatment, with long-acting injectables available for better adherence. Additional medications, such as antidepressants or mood stabilizers, may be used based on individual needs. Psychosocial approaches like therapy, social skills training, family support, and vocational rehabilitation enhance coping, communication, and daily life skills. Severe cases may require hospitalization for stabilization, while electroconvulsive therapy (ECT) is considered for those unresponsive to other treatments. With proper care, many people with schizophrenia can manage their symptoms effectively. (Mayo Clinic, n.d.) DIAGNOSIS Schizophrenia diagnosis involves a detailed psychiatric history and mental status examination, ruling out other potential medical and psychiatric causes of psychosis. Risk factors for developing schizophrenia include birth complications, being born in a specific season, maternal malnutrition, maternal influenza during pregnancy, a family history of the disorder, childhood trauma, social isolation, cannabis use, minority ethnicity, and living in urban environments (Messias, Chen, & Eaton, 2007; Davis et al., 2016). The exact cause and biological mechanisms of schizophrenia remain unclear due to its complexity and variability. Despite being relatively uncommon, schizophrenia has a significant impact on the global burden of disease, with more than half of those diagnosed experiencing multiple coexisting psychiatric and medical conditions (Chong et al., 2016). PRESCRIBED DRUGS First-Generation Antipsychotics First-generation antipsychotics (FGAs), also known as typical antipsychotics, primarily work by blocking dopamine receptors to alleviate symptoms of various mental health conditions. These medications are commonly prescribed for issues such as acute mania, agitation, and bipolar disorder. Some examples of FGAs include Chlorpromazine (Thorazine), Fluphenazine (Prolixin), Haloperidol (Haldol), and Loxapine (Loxitane), among others. (Mayo Clinic, n.d.) Mechanism: Both first- and second-generation antipsychotics block dopamine in the ventral tegmentum to reduce positive symptoms. However, first-generation drugs also affect the nigrostriatal dopamine system, leading to extrapyramidal side effects, which second-generation drugs cause less frequently. (Grace & Uliana, 2023) Efficacy: Studies revealed minimal differences in efficacy between First Generation Antipsychotics and Second Generation Antipsychotics, but haloperidol was less effective than amisulpride and clozapine. Additionally, olanzapine showed greater improvement in functional capacity compared to quetiapine and ziprasidone. (Pike et al., 2009) Second Generation Antipsychotics Second-generation antipsychotics (SGAs), also known as atypical antipsychotics, are newer medications that work differently from first-generation antipsychotics. Instead of fully blocking dopamine receptors, SGAs partially block them and may also influence other neurotransmitters like serotonin. Examples of SGAs include Aripiprazole (Abilify), Clozapine (Clozaril), Olanzapine (Zyprexa), Risperidone (Risperdal), and Quetiapine (Seroquel). (Mayo Clinic, n.d.) Mechanism: These medications inhibit some serotonin and dopamine receptors and stimulate other serotonin and dopamine receptors. (Cleveland Clinic, 2024) Efficacy: Patients with schizophrenia who were treated with SGAs showed significantly greater improvement in self-reported quality of life compared to those on FGAs, particularly when treatment was individualized. (Gründer et al., 2016) Side Effects: Studies show that olanzapine and risperidone are associated with the greatest weight gain, with olanzapine causing the largest increase in BMI. Paliperidone leads to the highest rise in total cholesterol but is the only drug to increase HDL cholesterol. Quetiapine XR shows the greatest reduction in fasting glucose, while lurasidone has the lowest weight gain, a reduction in BMI, and is the only treatment that decreases total cholesterol and triglycerides. Additionally, quetiapine XR is linked to the highest increase in both systolic and diastolic blood pressure. (Gründer et al., 2016b) Clozapine Clozapine is an FDA-approved atypical antipsychotic used for treatment-resistant schizophrenia. It is more effective than other antipsychotics for managing treatment-resistant schizophrenia and schizoaffective disorder. However, it is not the first-line treatment due to its potential for various adverse effects. (Haidary & Padhy, 2023) (Gammon et al., 2021) Mechanism: Clozapine acts as an antagonist by inhibiting dopamine D2 receptors and interacts with various serotonin receptors, such as 5-HT1A, 5-HT2A-C, 5-HT6, and 5-HT7.