Authors : Niharika Punia, Vikram A L, Shreya Ranjan,
Kanika Kushwaha.
UNDERSTANDING THE LINK BETWEEN CHILDHOOD TRAUMA AND SUBSTANCE ABUSE
ABSTRACT
Childhood trauma significantly impacts emotional regulation, self-worth, and coping mechanisms. Individuals often resort to self-medication with substances like alcohol and drugs to numb overwhelming emotions such as fear and sadness. Prolonged exposure to trauma disrupts the body’s stress response, leading to chronic anxiety and irritability. Additionally, early attachment disruptions hinder the development of healthy emotional bonds, resulting in persistent attachment issues. Experiences of abuse and neglect contribute to low self-esteem and feelings of unworthiness, making individuals more vulnerable to substance use as an escape. Addressing these challenges through therapeutic interventions is crucial for healing and resilience.
INTRODUCTION
Childhood trauma has lasting effects on emotional and psychological well-being, often leading to substance abuse as a coping mechanism. The self-medication hypothesis suggests that individuals with early-life trauma turn to alcohol or drugs to manage distress (Garland et al., 2013). Additionally, childhood adversity alters neurobiological pathways and attachment systems, increasing the risk of addiction. Understanding this connection is crucial for developing effective interventions that address both trauma recovery and substance dependency.
KEYWORDS: Childhood trauma, Substance abuse, Mental health, Trauma recovery, Childhood adversity, Addiction, Psychological distress, Coping mechanisms, Self-medication, Emotional healing.
DISCUSSION
SELF-MEDICATION AND ESCAPING EMOTIONAL PAIN
Individuals who experience childhood adversity often use substances as a form of self-medication to ease psychological distress. The emotional pain from early-life trauma can cause heightened anxiety and stress, leading individuals to seek temporary relief through alcohol or drugs. While substances may offer short-term comfort, they often create a cycle of addiction, increasing dependency over time (Abhasa, n.d.; Garland et al., 2013).
Studies show that trauma history significantly contributes to psychological distress, often leading to substance misuse. A study involving at-risk youth found that exposure to traumatic life events creates a feedback loop where emotional distress fuels substance abuse, worsening mental health over time (Garland et al., 2013). This pattern highlights how unresolved trauma can lead individuals to depend on substances for emotional regulation.
Childhood trauma also affects the brain’s reward system, which plays a critical role in addiction. Trauma disrupts the ability to regulate dopamine, the chemical responsible for pleasure and reward. This makes individuals more susceptible to the reinforcing effects of substances like alcohol or drugs, which artificially elevate dopamine levels (Abhasa, n.d.; Harris House, 2018).
Additionally, emotional dysregulation, a common consequence of childhood adversity, increases the risk of substance use disorders. Individuals struggling to manage intense emotions often turn to substances as a coping mechanism. This reliance is dangerous, as substances provide temporary relief but prevent the development of healthier coping strategies (Harris House, 2018).
THE PHYSIOLOGICAL AND PSYCHOLOGICAL EFFECTS OF TRAUMA
Childhood trauma, especially when experienced over extended periods, can have lasting effects on an individual’s ability to cope with stress. The body’s natural response to stress is governed by the hypothalamic-pituitary-adrenal (HPA) axis, which plays a crucial role in regulating the release of stress hormones, particularly cortisol. When a stressor is perceived, the hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH). This hormone then prompts the adrenal glands to produce cortisol, a key stress hormone. Cortisol helps improve energy levels, modulate immune responses, and maintain homeostasis. Once the stressor is resolved, cortisol levels should decrease, signalling the hypothalamus to reduce CRH production, thus restoring balance to the system (Bremner, 2006). When a child is exposed to traumatic experiences, such as abuse or neglect, the HPA axis can become chronically activated, leading to a state of heightened arousal and stress.
This chronic activation can disrupt the body’s internal equilibrium, making it difficult for individuals to return to a state of calm after experiencing stress. As a result, the body may remain in a constant state of alertness, which can have profound implications for both mental and physical health (Noushad et al., 2021). The phrase “the mind forgets, but the body keeps the score” encapsulates this phenomenon, highlighting how trauma can manifest in physical symptoms and health issues long after the initial events have passed.
The dysregulation of the HPA axis can lead to a range of psychological conditions, including anxiety and depression. In some cases, individuals may experience overactivity of the HPA axis, resulting in excessive cortisol production, which can contribute to symptoms such as insomnia, irritability, and heightened anxiety. Conversely, some individuals may experience underactivity of the HPA axis, leading to insufficient cortisol levels, which can result in fatigue, low mood, and difficulty coping with stress (Chrousos Philip W., 1992). Children who experience trauma frequently struggle with emotional regulation. They may exhibit behaviours such as impulsivity, aggression, or difficulty calming down after distressing experiences. It can also influence how individuals perceive threats, increasing the likelihood of developing anxiety disorders and PTSD (Dorn George P., 1993).
Moreover, the effects of childhood trauma extend beyond psychological symptoms. Chronic stress and HPA axis dysregulation can contribute to various physical health issues, including cardiovascular disease, obesity, and autoimmune disorders (Steptoe & Kivimäki, 2012).
The interplay between mental and physical health underscores the importance of addressing the effects of childhood trauma holistically. Supportive caregiver relationships have been shown to mitigate some of the adverse outcomes associated with childhood trauma by enhancing emotional processing and reducing threat sensitivity (Folkman, 1984).
ATTACHMENT ISSUES AND DEPENDENCY ON SUBSTANCES
Attachment theory suggests that early relationships shape an individual’s ability to form secure connections in adulthood. When childhood trauma disrupts this process, it can result in insecure attachment styles, such as fear of abandonment, neglect, or rejection. These insecurities often make individuals more vulnerable to substance dependence as they seek maladaptive coping mechanisms (The Guest House Ocala, 2023; International Journal of Indian Psychology, 2024).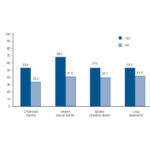
Fig. 1 Association between childhood traumatic experiences and lifetime cannabis use (Tomassi S et al., 2017).
For example, individuals with anxious or avoidant attachment styles may use substances to suppress emotions related to relational insecurity or low self-worth. Insecure attachment has been linked to mental health disorders and substance use disorders (SUDs). When individuals lack a secure base, they often develop negative expectations about relationships, leading to self-soothing behaviours such as substance abuse (The Guest House Ocala, 2023).
The long-term impact of attachment trauma includes persistent relationship struggles and dependency on substances. This highlights the need for comprehensive treatment that addresses both trauma recovery and addiction therapy. Trauma-focused cognitive-behavioural therapy (CBT) and eye movement desensitization and reprocessing (EMDR) are effective in helping individuals process emotional pain without substances(Abhasa, n.d.; International Journal of Indian Psychology, 2024).
Furthermore, addressing relational dynamics in treatment is crucial, as attachment insecurities often contribute to addiction. Family-based therapies and interventions that rebuild trust and communication play a significant role in overcoming trauma (The Guest House Ocala, 2023). When individuals establish healthy emotional connections, they are less likely to rely on substances for comfort.
THE CONNECTION BETWEEN SUBSTANCE ABUSE, SELF-WORTH, AND CHILDHOOD TRAUMA
A person’s view of themselves can be seriously distorted by childhood trauma, which includes emotional neglect, physical abuse, and exposure to dysfunctional households. These negative experiences frequently result in internalised emotions of guilt, worthlessness, and inadequacy that last well into adulthood. Frequent exposure to these stresses interferes with the normal development of emotional control and self-worth, making people more vulnerable to psychiatric problems in later life. Because unresolved trauma frequently shows up as poor self-esteem and negative self-perceptions, research indicates that adverse childhood experiences (ACEs) are intimately linked to the development of long-term emotional discomfort (Nelson et al., 2017). Adversities in early childhood change emotional resilience and raise the risk of developing unhealthy coping strategies as an adult.
Given that people with unresolved trauma often use drugs as a kind of self-medication, the link between substance use and early trauma is especially strong. By numbing emotional anguish, substances give momentary respite from overpowering emotions of guilt and poor self-worth. However, the cycle of trauma and addiction is frequently reinforced by this maladaptive coping mechanism, making recovery more challenging. Research shows that vulnerability to drug use disorders is increased by dysregulation of the stress-response system, which is frequently brought on by childhood trauma (Khoury et al., 2010). Breaking this pattern and fostering long-term healing requires addressing the underlying causes of trauma and offering trauma-informed treatment.
Childhood trauma has an impact on parenting and family relations, affecting not only the person but also subsequent generations. Traumatised people frequently have trouble controlling their emotions and forming healthy relationships, which can make it difficult for them to give their kids safe, supportive surroundings. According to research, generations of emotional instability and inadequate coping strategies are sustained by unresolved trauma. Due to unresolved psychological issues, parents with a history of trauma may unwittingly expose their kids to comparable hardships, such neglect or emotional invalidation. Family-based therapies and trauma-focused therapy are necessary to break this pattern because they address underlying issues, build resilience, and encourage better connections. According to ( Schofield et al. 2011), trauma-informed techniques are essential for reducing the long-term, intergenerational impacts of childhood adversity.
CONCLUSION
The link between childhood trauma and substance abuse highlights the importance of trauma-informed treatment. Self-medication, neurobiological disruptions, and insecure attachment styles contribute to addiction, reinforcing a harmful cycle. Effective interventions should integrate trauma-focused therapies and relational healing to promote long-term recovery. Future research should explore early interventions to prevent substance use disorders. Addressing both the psychological and physiological effects of childhood adversity is crucial for breaking the cycle of addiction and fostering resilience.
References:
Abhasa. (n.d.). Childhood trauma and addiction: A complex relationship. Retrieved from https://www.abhasa.in/articles/link-between-childhood-trauma-and-addiction/
Bremner, J. D. (2006). Traumatic stress: effects on the brain. Dialogues in Clinical Neuroscience, 8(4), 445. https://doi.org/10.31887/DCNS.2006.8.4/JBREMNER
Chrousos Philip W., G. P. ; G. (1992). The Concepts of Stress and Stress System Disorders: Overview of Physical and Behavioral Homeostasis. JAMA, 267(9), 1244–1252. https://doi.org/10.1001/jama.267.9.1244
Dorn George P., L. D. ; C. (1993). The endocrinology of stress and stress system disorders in adolescence. Endocrinology and Metabolism Clinics of North America, 22(3), 685–700. https://doi.org/10.1016/s0889-8529(18)30158-0
Folkman, S. (1984). Personal control and stress and coping processes: A theoretical analysis. Journal of Personality and Social Psychology, 46(4), 839–852. https://doi.org/10.1037/0022-3514.46.4.839
Garland, E. L., Pettus-Davis, C., & Howard, M. O. (2013). Self-medication among traumatized youth: Structural equation modeling of pathways between trauma history, substance misuse, and psychological distress. Journal of Behavioral Medicine, 36(2), 175–185. https://doi.org/10.1007/s10865-012-9413-5
Harris House ST. Louis. (2018). How childhood trauma contributes to adult substance abuse. Retrieved from https://harrishousestl.org/how-childhood-trauma-contributes-to-adult-substance-abuse/
International Journal of Indian Psychology. (2024). The relationship between childhood trauma, coping mechanisms, and substance abuse among young adults. Retrieved from https://ijip.in/wp-content/uploads/2024/05/18.01.143.20241202.pdf
Khoury, L., Tang, Y. L., Bradley, B., Cubells, J. F., & Ressler, K. J. (2010). Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depression and Anxiety, 27(12), 1077-1086. https://doi.org/10.1002/da.20751
Nelson, J., Klumparendt, A., Doebler, P., & Ehring, T. (2017). Childhood maltreatment and characteristics of adult depression: Meta-analysis. British Journal of Psychiatry, 210(2), 96-104. https://doi.org/10.1192/bjp.bp.115.180752
Noushad, S., Ahmed, S., Ansari, B., Mustafa, U.-H., Saleem, Y., & Hazrat, H. (2021). Physiological biomarkers of chronic stress: A systematic review. International Journal of Health Sciences, 15(5), 46–59.
Schofield, G., Lee, P., & Merrick, M. T. (2011). The intergenerational transmission of childhood adversity: Evidence, implications, and interventions. Child and Family Social Work, 16(4), 398-409. https://doi.org/10.1111/j.1365-2206.2011.00719.x
Steptoe, A., & Kivimäki, M. (2012). Stress and cardiovascular disease. Nature Reviews Cardiology, 9(6), 360–370. https://doi.org/10.1038/nrcardio.2012.45
The Guest House Ocala. (2023). How does attachment trauma connect to addiction? Retrieved from https://www.theguesthouseocala.com/how-does-attachment-trauma-connect-to-addiction/