By Mrunmai Thakur, Amreena Manzoor, Saumya Tomar, Nahela Khan.
Introduction
The world accommodates 8.23 billion people—and with such a vast population we are landing
on the moon, creating masters in the AI Sector, making our lives more luxurious than ever
before.
But amidst all these advancements, do you know how many people are still suffering from
POVERTY?
Approximately 8.5% of the world is still battling the harsh reality called POVERTY. These
individuals are struggling to meet even the most basic necessities —Food, Shelter and Clean
Water.
In 2024, Sub-Saharan Africa accounted for 16 % of the world’s population but shockingly, it
housed 67% of the people living in extreme poverty. This is not just an economic problem— it’s
a health disaster.
Poverty significantly impacts global health, leading to shorter lifespans, higher infant
mortality, and increased susceptibility to diseases, particularly in marginalized communities,
due to lack of access to quality healthcare, nutritious food, and safe living
conditions. Families affected by poverty often have to make impossible choices selling of assets
to afford medical care, borrowing money at high interest rate, or falling into deeper debt.
In this article we will dive into the crucial relationship of Poverty and Health, and we will
explore:
● How poverty affects both physical and mental health
● The deep-rooted presence of poverty across different parts of the world
● Case studies that reflect real-world consequences and outcomes
● Thoughtful strategies and insights that can help us not completely eradicate—but
significantly minimize—poverty and its painful effects.
Together let’s shed light on this crisis that continues to make lives miserable in a world full of
progress.
Physical Health effects
Malnutrition:
Malnutrition, in all its forms, includes undernutrition (wasting, stunting, underweight),
inadequate vitamins or minerals, overweight, obesity, and resulting diet-related
noncommunicable diseases.In 2022, 2.5 billion adults were overweight, including 890 million who were living with obesity, while 390 million were underweight. Every country in the world
is affected by one or more forms of malnutrition. Combating malnutrition in all its forms is one
of the greatest global health challenges.Women, infants, children, and adolescents are at
particular risk of malnutrition.In 2024, globally, around 733 million people faced hunger, and
almost 5 million children under age 5 died, with nearly half of these deaths linked to
undernutrition, according to the UN’s State of Food Security and Nutrition in the World
report. Increased susceptibility to diseases due to poor living conditions.
Increased susceptibility to diseases due to poor living conditions:
Poverty and poor health worldwide are inextricably linked. The causes of poor health for
millions globally are rooted in political, social and economic injustices. Poverty is both a cause
and a consequence of poor health. Poverty increases the chances of poor health. Poor health, in
turn, traps communities in poverty. Housing is a social determinant of health. A safe house
away from potential hazards can promote well-being. However, living in unsafe or unsuitable
housing conditions may contribute to health inequities and be a factor in health problems, such
as chronic diseases. Due to poverty increase the huge amount of people do not have access to
proper sanitation leading to hazardous diseases which are life threatening.
Lack of access to healthcare and medical services:
Sub-Saharan Africa is widely considered the poorest region in the world, with a significant
portion of its population living in extreme poverty and facing numerous challenges related to
development, governance, and conflict. Health systems in SSA are generally considered
vulnerable, and they find it difficult to adapt to changing health conditions. Inadequately skilled
healthcare professionals, underfunding, poor knowledge, the absence of governance and
leadership, lack of transparency and bureaucracy are the main preparedness barriers due to poor
detection and response systems, every year, many SSA countries experience major public
health events with a significant risk of a rapid spread. A good example is the Ebola virus
epidemic which struck some West African countries in 2014. This public health event has
exposed the vulnerability of the population, the economy, and the poor capacities of the affected
countries to anticipate and cope with health disasters.
Mental health and Poverty
The relationship between poverty and mental health has been overlooked and it’s worth
emphasizing. Those with the lowest incomes in a community suffer 1.5 to 3 times more
frequently from depression, anxiety and other common mental illnesses from those with the
highest incomes. For instance: in India, 3.4% of those in the lowest income quintile
experience depression at any given time, compared with 1.9% of those in the highest
quintile. (Fig 3)
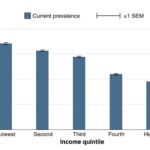 Fig. 3 Prevalence of depression by income quintile in India. The average percentage of people
Fig. 3 Prevalence of depression by income quintile in India. The average percentage of people
in each income quintile in India who have had depression within the past 2 weeks (“current”
prevalence).
These numbers come from an analysis of the Indian Mental Health Survey 2015-16.
There exists a bidirectional relationship between the two. Mental health problems are both the
cause and consequence of poverty. The economic loss due to mental health conditions in
India, between 2012-2030 is estimated at USD 1.03 trillion, the World health organization
says. Lack of proper housing and exposure to environmental stressors such as climate change,
pollution can worsen mental health. The Homeless Mentally ill (HMI) are the most neglected
and vulnerable section of the society with many surveys finding it difficult to quantify them
reflecting lack of awareness and rehabilitation facilities. A wide variety of illicit drugs, alcohol,
tobacco and other substance use disorders (SUDs) is prevalent among the poor and their use
among the youth is a growing concern. The National Mental Health survey 2015-16 observes,
“Stress relief, curiosity, recreation, lack of family support/ emotional support for youths and
depression were some of the reasons brought out by participants in many states.” The impact of
substance abuse is not only detrimental to the individual but also severely affects their families
with financial loss, lack of peace, negative impacts on children, violence and stressed
relationships. There is a higher prevalence of depressive disorders, bipolar and
post-traumatic stress disorders among such individuals (both male and female).The social
stigma surrounding poverty leading to humiliation, discrimination and reinforced prejudices, serves detrimental to the individuals who then feel a loss of pride and dignity. Such
psychological stressors increase the likelihood of mental health problems thus continuing the
cyclical link.
Treatment gap in India remains high- The relationship between poverty and mental health
becomes even more pertinent after the pandemic with India spending as little as 0.06% of its
budget on mental health, and only 0.3 psychiatrists per 100,000 people in the country. The
demand-side barriers and supply side barriers need to be examined.
 Fig 4 Mental Health Expenditure by country income category. The average percentage of
Fig 4 Mental Health Expenditure by country income category. The average percentage of
overall health budgets spent on mental health across countries in each of the four income
categories used by the World Bank.
A key barrier in the demand side attributed to a wider treatment gap for mental health is the low
perceived need for mental-health related treatments due to limiting socio-cultural beliefs and
social stigma. The poor are more likely to visit traditional healers or associate it with black
magic rather than a medical condition. Significant supply side barriers include inadequate
training for public health-care professionals, inability to diagnose or manage mental health
disorders. Creating public awareness on mental health, active community engagement alongside
strengthening the health system’s action plan such as scaling up existing services (District
Mental Health Program), developing innovative mental health services to reach the
underprivileged section in the country is necessary to narrow the treatment gap for mental health.
Case Study and Data
Poverty and health create a vicious cycle. Poor health minimizes income, while poverty restricts
access to healthcare and nutrition, worsening health issues. According to the Global
Multi-dimensional Poverty Index released by the United Nations Development Program
(UNDP) and Oxford Poverty and Human Development Initiative (OPHI), these
organizations released this report which evaluates data from over 110 Developing countries,
Multidimensional poverty deals with indicators such as health, education, quality of life and
assets. This survey points out that 1.1 billion people in the world are still living below the
poverty line. In the case of India for example, in (2005-6) 55% of our population was below the
poverty line by (2015-16) it came down to 27.7%, and by (2019-21) it came down to 16.4% and
similarly, improvements are made by other countries as well.
Poverty remains concentrated in Sub-Saharan Africa where 53.4 crores of the 110- crore
people live below the poverty line. This area faces severe public health challenges, including
high child mortality, malnutrition, and infectious diseases. Nigeria, the largest country in the
region, exemplifies the consequences of poverty, with 37% of children stunted due to chronic
malnutrition. The under-five mortality rate remains high in deprived areas.
In the context of South Asia, 38.9 crores live below the poverty line and about 23 crores reside
in India. Poverty in Bihar creates a barrier to accessing healthcare services, especially in rural
areas where healthcare facilities are either inadequate or non-existent. According to a 2018 study
by the Lancet, only 40% of the rural population in Bihar had access to essential healthcare
services. Long distances, poor roads, and the high cost of medical treatment prevent many
families from seeking care until health issues become life-threatening, In recent years the
government of India is working to improve maternal and child health care services by increasing
the availability of public health clinics.
In India 41. 5 crore people have moved out of poverty between 2005-6 and 2019-21, The
Intensity of poverty is also declining showing a reduction in the amount of deprivation among
poor populations in states such as Bihar, Uttar Pradesh, Madhya Pradesh, Odisha and
Rajasthan recorded a faster decline in poverty levels indicating a reduction in disparities among
population.
Possible Strategies and Solutions
Good healthcare services can help people in getting out of poverty and thus build a more stable
and prosperous nation. There are various ways to achieve it-:
● First, developed countries should transfer expertise and economic resources to develop
healthcare infrastructure in developing countries. (Alqassim & El-Setouhy, 2022)
● Second, with the collaboration between NGOs and government agencies, mobile clinics
and community health centers can be set up to provide healthcare services in rural areas.
The NGOs have expertise and grassroots understanding while the government has
resources and power. (Doshmangir, Sanadghol, Kakemam, & Majdzadeh, 2025)
● Third, subsidized public health insurance is necessary to cover out-of-pocket expenses,
especially in a situation when people in rural areas often sell assets or take loans to afford
medical care. The Rashtriya Swasthya Bima Yojana (RSBY) and Ayushman Bharat
Scheme in India are beneficial, but they struggle with challenges like quality health care,
lack of awareness, maintenance of data, digital divide and capacity building. Thus, a
well-planned and executed public health insurance policy is the need of the hour.
● Fourth, for the mental health crisis, there can be 3 levels of intervention: intervention
from a family perspective by giving them emotional and material support; from a school
perspective by including courses like emotional learning, resilience, life skills and
character education in the curriculum; and from a public health perspective, where mental
health is taken into account in policies and practices meant for reducing poverty. (Sun,
2023)
● And at last, the fifth possible solution is related to the factors that influence public health
and are mostly found in the social and economic development space, like adequate
housing, food security, clean water availability, environmental exposure and
transportation. Hence, there is a need to work on all these, as all social policy is health
policy.
In conclusion, while poverty continues to limit access to essential resources, progress is being
made to improve those affected lives. Efforts to reduce malnutrition, improve housing, and
address preventable diseases are essential in health. In Africa focusing on sustainable
development, a Nutritious diet, and better living conditions is key to building a bright future.
There is a need to increase awareness and improve mental health infrastructure by addressing
economic hardship reducing stigma and providing accessible care that will improve both
physical and mental well-being. Collaboration between government, NGOs, and communities to
create solutions that uplift those in poverty. We can work towards a healthier, more equitable
world for all.
References:
● WorldHealthOrganization.(2023,December13). Malnutrition.
https://www.who.int/news-room/fact-sheets/detail/malnutrition
● Cherney, K. (2023, October 17). Housing and health: What’s the connection?
Medical NewsToday
https://www.medicalnewstoday.com/articles/housing-and-health#impact-of-housing
on-health.
● Outreach International. (2023, September 26). Understanding poverty in Africa:
Causes, effects & solutions.https://outreach-international.org/blog/poverty-in-africa/ –
● Alqassim, A. Y., & El-Setouhy, M. (2022). Impact of poverty on health. Healthcare Access New
Threats, New Approaches.
https://www.researchgate.net/publication/365809771_Impact_of_Poverty_on_Health2-4.
● Sun, Y., 2023. The Effects of Poverty on Mental Health and Interventions. SHS Web of Conferences
157.2-4
https://www.shs-conferences.org/articles/shsconf/abs/2023/06/shsconf_essc2023_01022/s
hsconf_essc2023_01022.html
● Doshmangir, L., Sanadghol, A., Kakemam, E., & Majdzadeh, R. (2025). The
involvement of non-governmental organisations in achieving health system goals
based on the WHO six building blocks: A scoping review on global evidence. Plos
One. 9-11. https://pmc.ncbi.nlm.nih.gov/articles/PMC11781716/
● UNDP – Global Multi-dimensional Poverty Index
https://r.search.yahoo.com/_ylt=Awr1QNuSzfJn.lIFLhPnHgx.;_ylu=Y29sbwMEcG9zAz
EEdnRpZAMEc2VjA3Ny/RV=2/RE=1743994387/RO=10/RU=https%3a%2f%2fhdr.und
p.org%2fcontent%2f2024-global-multidimensional-poverty-index-mpi/RK=2/RS=kHf_V
EMrNN7Iyi4NwLw27dBgIWA-
● National Mental Health Survey of India, 2015-16: Prevalence, Patterns and
Outcomes. Bengaluru, National Institute of Mental health and Neuro Sciences,
NIMHANS Publication no. 129, 2016
https://indianmhs.nimhans.ac.in/phase1/Docs/Report2.pdf